
In this blog post, we’ll delve into the realm of HL7 interfaces, providing you with a comprehensive understanding of what HL7 is, how HL7 integration works, and why HL7 interfaces and HL7 software are game-changers in the world of healthcare data integration. Whether you’re a seasoned healthcare professional or just curious about the ins and outs of the industry, we’re here to demystify the world of HL7 and showcase its transformative potential.
HL7’s latest standard is known as Fast Healthcare Interoperability Resources, abbreviated as HL7 FHIR (pronounced as “fire”). HL7 FHIR establishes a shared vocabulary for the exchange of healthcare data and enables the structured organization of information through a hierarchical coding system.
FHIR is designed to be simpler and more accessible than previous standards. It uses modern web standards, such as JSON and XML, making it easier for developers to work with.
FHIR is modular, meaning it can be used in parts. This allows for gradual adoption and integration with existing systems, reducing the need for a complete overhaul.
Why HL7 integration has become a necessity in the digital age?
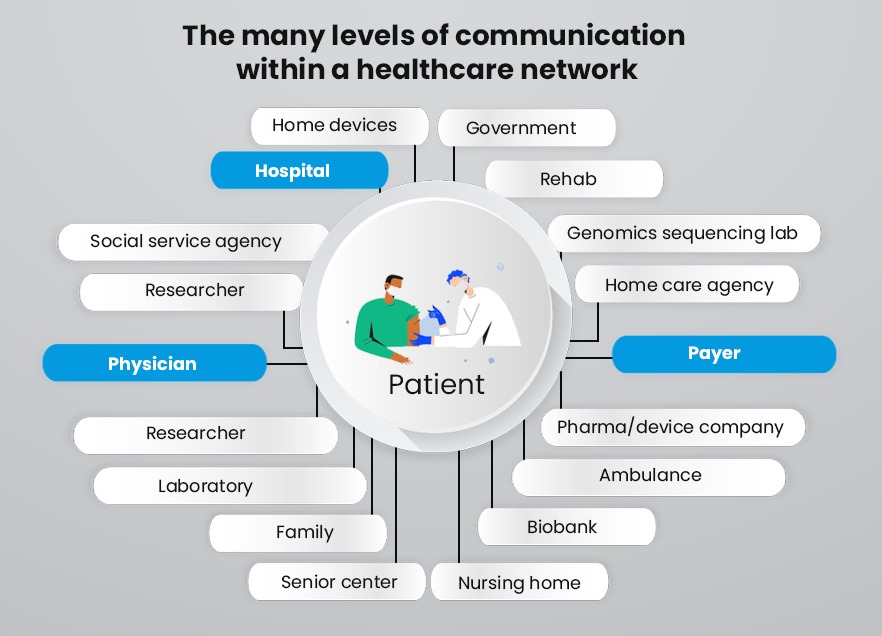
HL7 standards were a leap in the right direction for healthcare providers. Lack of system interoperability was costing US Healthcare systems an annual loss of almost 30 billion USD. Every healthcare provider has numerous specialized applications that interact with each other, right from billing, to diagnostics, to patient records. Since these applications are usually developed by different vendors, they might be built in different languages and platforms. That causes a block when it comes to different systems sending data to each other.
Let alone applications being unable to talk to each other seamlessly within one hospital or healthcare facility, the problem was compounded when two different healthcare providers needed a health information exchange of their data. Communication between different types of software has been hard to achieve before the development of common standards provided by HL7 protocols.
Health Level-7 or HL7 has been developed by Health Level 7 International, a not-for-profit organization. The advantage of the HL7 standard is that when a majority of healthcare software incorporates it, interoperability eases the exchange of healthcare data without having to resort to special software for conversion. So whether you are located in India, the UK, or the USA – it follows the same framework and similar standards.
WHat is HL7 standards?
HL7 standards, a foundational concept in healthcare informatics, are the bedrock upon which the HL7 interface and HL7 integration are built. These standards play a pivotal role in ensuring seamless communication and data exchange among various healthcare systems and software applications.
HL7, which stands for Health Level 7, is a set of international standards developed by the HL7 International organization. These HL7 interfaces are designed to facilitate the sharing of clinical and administrative data across different healthcare entities, such as hospitals, clinics, laboratories, and more.
These HL7 standards define a common language and structure for healthcare data, ensuring that information is exchanged accurately and consistently. By adhering to HL7 standards, healthcare organizations can achieve interoperability, streamline processes, and enhance patient care.
In essence, understanding what is HL7 in Healthcare and how it can be implemented is crucial for healthcare organizations in America.. This starts with HL7 integration into EHR systems, and the broader application of HL7 software in healthcare. These standards form the backbone of data sharing, making it possible for disparate systems to communicate effectively and, in turn, answering the question of how HL7 is used in healthcare to enhance overall patient outcomes.
How is HL7 used in healthcare?
Electronic Health Records (EHRs) and interoperability are the two major drivers of technology in the healthcare segment. Interoperability is where the use of HL7 is highly significant.
To quickly understand how HL7 works, you can relate it to the process of the Internet linking millions of websites. Each of them might be developed using different languages such as PHP, .NET or WordPress (among many other platforms) but all follow the same W3C standards. Similarly, HL7 protocols define a framework that governs how electronic health data can be retrieved, shared as well as integrated.
HL7 uses a number of standards such as application standards, messaging standards, etc. that follow a set of HL7 protocols for packing and communicating between different systems. It achieves this by defining the language, data type as well as structure of the data and how it must be packaged. More than 90% of the major healthcare facilities in the US use HL7 and it’s widely adopted in over 27 countries, making it a truly global standard. Many healthcare organizations turn to HL7 integration specialists like iTech India, to integrate various existing systems and interfaces that are already running in a hospital or medical facility and also correct the prior HL7 implementation outcomes.
The HL7 standard has 2 different versions – Version 2 and Version 3. The 2.3 or 2.3.1 are most commonly used while V3 has only a smaller usage since it is not backward compatible with systems using the V2 version.. HL7 is now working on HL7 FHIR (Fast Health Interoperable Resources) which will be easier to implement since it uses modern API technology. APIs (application programming interface) is driving digital transformation outside of healthcare but there are some cybersecurity concerns which is inhibiting its wider adoption in Healthcare.
Benefits of HL7 interface integration
The US healthcare industry is particularly heavily regulated and the large amount of medical data that is continuously generated makes the industry even more complex. A common framework for data communication brings with it many benefits, let’s dive into the leading benefits.
1. Ensuring data uniformity
Statistical studies indicate that each patient contributes 80 megabytes of EMR and imaging data every year. This is a mountain of data when you look at the exponential increase of the cumulative total of patients in the system. While EMR is limited to a single medical practice, an EHR is a digital record from multiple doctors and is a holistic long-term view of the patient’s health. This is a clear indication of how important it is that health data cannot be isolated and sit in different pools.
By ensuring data uniformity between different applications within and between medical facilities, allows patient information and other health information exchange to be seamlessly transferred from admission to diagnostics, to treatment and billing.
2. Automation of workflows
Manual data entry is time-consuming and automation of repetitive tasks is both an energy and cost saver. A standardized HL7 data workflow can help synchronize data updates simultaneously. For instance, records, lab tests, and prescriptions exchanged between departments can completely eliminate manual data entry.
3. Facilitate information exchange with regulators
Healthcare providers, in the US particularly, need to regularly share information with regulators to meet public health reporting standards. When medical systems achieve HL7 compliance, it can simplify this process and reduce the burden on admin by sharing data electronically. This is particularly important when it comes to medical devices sharing their specifications. The same for biopharmaceuticals that need to share information about drug development and clinical trials.
4. Facilitates collaboration globally
With over 27 countries and 1600 healthcare providers having adopted the HL7 standards, for the first time in history, it has become easier to share medical data across borders. This international collaboration has been of crucial importance in the global Covid-19 pandemic.
5. Patients can conveniently access their records
When EHR records are coupled with interoperability, patients will be able to access their records and new updates easily online. This becomes a boon when it comes to consulting multiple specialists. The time-consuming process of lugging around a pile of documents or providing a full picture of their medical history is instantly solved.
6. Reduce investments in new technology upgrades
While investing in adding a new HL7 framework will require an initial investment, the costs reduce in the long run. This is because the system life of legacy systems can be extended since it uses the messaging services of the HL7 framework to interface with newer systems.
Need Help with your HL7 implementation?
iTech’s HL7 Connect is a proprietary product that provides a threefold advantage – It’s practical, cost-effective, and HL7 compliant. We have over 10 years of building healthcare solutions for the US and India. If you are reading this, you are ready for the benefits of an HL7 interface, contact iTech India today.








