
Digital technology is so interwoven into our lives that we cannot easily remember a world where information was not available to us 24/7. Yet, imagine a world where we could not speak to someone because they had a different mobile service provider than ours. Even more outlandish would be if we could not send out an email to someone with a different email service. The reason that communication is easy is because interoperability is a standard for all services. Yet, when we come to electronic medical records, this might not be wholly true.
Electronic health records are not a more efficient replacement for paper-based patient records. It goes much deeper than that. For the first time patient medical records moved towards a standardized format that is designed to be sharable with other healthcare providers to ensure the highest level of continuity of care. And this is exactly why patient digital records cannot sit within a single medical practice on in-house servers. It then follows that hospitals and even smaller practices that have invested in server-based EHR software systems now need to migrate to cloud-based EHR software . However, not all are ready to make a hefty investment in a complete migration. So is there another interim solution where in-house systems can still communicate with other services on the cloud?
Types of EHR software systems
There are essentially two types of EHR systems and this is based on where the servers which store the data are located:
1. Physician hosted: This means that the medical practice has purchased the hardware as well as the software along with the licenses to handle it. A Client-based server means that the practise is responsible for the data security as well as maintenance. An alternate to this could be if the data is stored on the vendor’s dedicated servers. Either way, the healthcare provider will enter into a contract with the vendor to handle this. This category of EHRs though have found fewer takers in the modern world, with most migrating to a cloud-based EHR for interoperability in healthcare that also brings cost benefits.
2. Cloud-based EHR: More than two-thirds of healthcare providers have moved to the cloud and the reasons are many. A cloud-based solution for electronic health record software is scalable, flexible, improves interoperability in healthcare and is also a cost-effective way to maintain patient health files in the cloud rather than on internal servers located in large server rooms in a medical facility. Cybersecurity is outsourced to the company that makes the EHR and upgrades become the responsibility of the platform provider. This allows medical facilities to focus on ther IT needs rather than data center management.
iTech in our EHR implementation process for smaller medical practices (11 clinicians or less) have found that smaller the practise, the less likely they are to use advanced technology tools and this is why they are frustrated with their existing EHR systems. Most larger facilities have already switched to a cloud-based EHR system because they have had issues with health data exchange with their older systems. However, smaller practices who have already invested in EHR albeit desktop versions are reluctant to do a complete migration in one-go. Yet, they still need to leverage interoperability with other healthcare providers. iTech has worked with many such healthcare facilities to create an interface between internal and external systems.
What is interoperability in healthcare and the inherent challenges
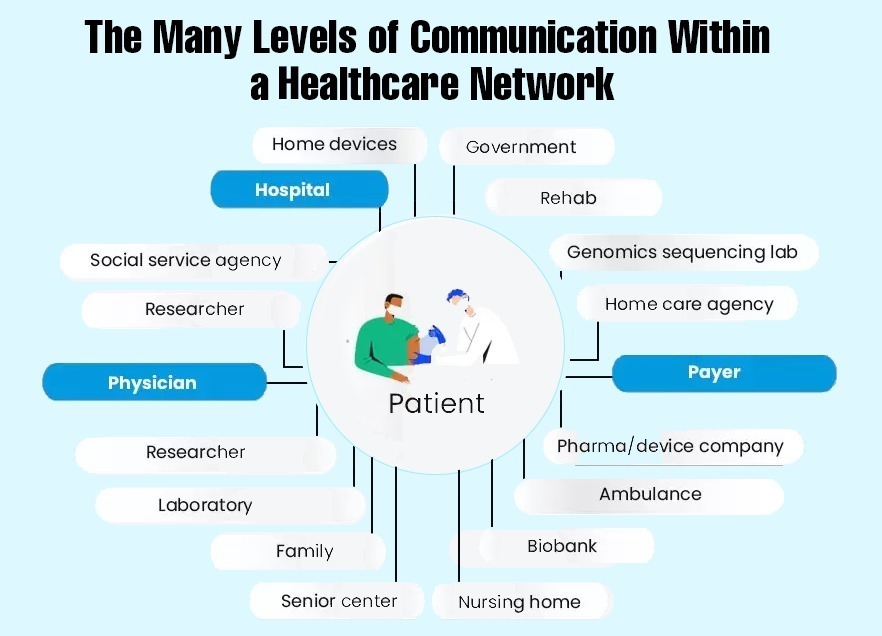
In its simplest term, interoperability is the ability of a system to be integrated with any other system to share information. In the medical mileu, EHR interoperability is the necessity for information to be seamlessly shared between care-providers and all other healthcare systems that are involved in the care delivery for a patient.
Interoperability is the ability of a system to be integrated with any other system to share information.
The Office of the National Coordinator for Health Information Technolgy (ONC) has set down the interoperability standard advisory (ISA) that must be followed to recognize an EHR platform to be interoperable. It refers to the ease with which healthcare information and medical records can be shared or transferred between one system and another. This requires 4 technologies to be integrated:
● Application interaction with authorised users
● System communication
● Information processing and management
● Consumer device integration
Why is sharing data so difficult in the medical world? Let’s look at in the context of Spain and Portugal sharing the same language. However, in Spain, the word “propina’’ has a positive connotation as in a ‘tip’ as recognition of services. In Portugal though ’propina’ means a bribe. SImilarly, in health data, a patient can be identified as “Jack Miller” in one system and in another it could be “Miller Jack”. In America, there is no universal standard that 100% accurately identifies patients and so there is no consitency in matching them to all their medical records.
We have the technology!
Communication between different types of software, has been difficult to achieve before the development of Health Level 7 or HL-7 standard (developed by Health Level 7 International, a not-for-profit organisation). The difficulty arose because software from different vendors are written in different programming languages and use different data types and file formats for information storage.
Of course, newer systems follow the HL-7 protocols i.e. a set of standards such as application standards, messaging standards etc. These standards for packing and communicating information between different systems is easy when it is put in place from the start. But this is not the case for systems developed prior to the global acceptance of the HL-7 standards.
So, what is the solution for these older systems that need to have HL-7 implemented, yet investing in a wholly new platform might not be the route they wish to take? System interoperability though is a necessity especially since healthcare providers in the US need to share information with regulators to meet public health reporting standards.
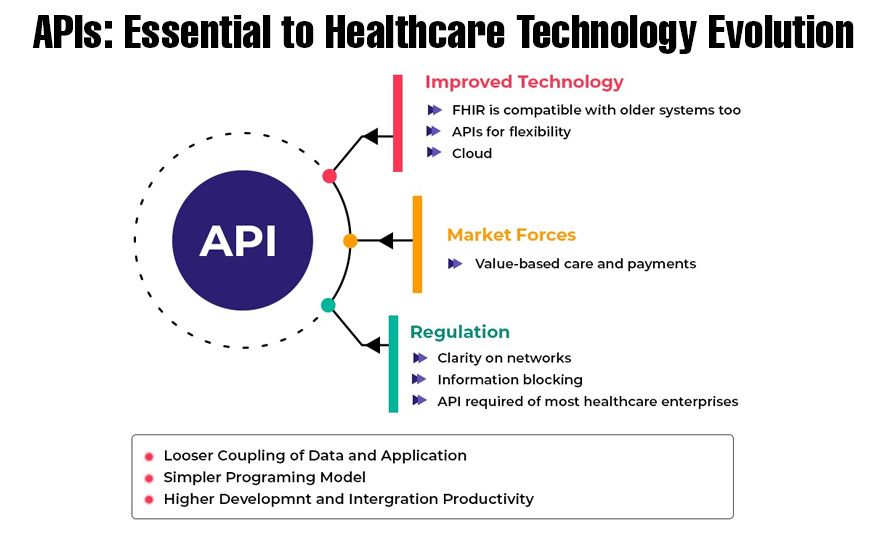
APIs in healthcare (Application Programming Interfaces) allow information systems to communicate and transfer data back and forth from one system to another.
iTech India healthcare solutions is a transformation hub where healthcare software challenges find solutions. iTech has implemented solutions for dental and physician practices as well as smaller medical healthcare providers who have identified themselves as wanting interoperability but being held back by their current systems.
Our proprietary product HL7 Connector builds and implements an interface between existing systems that is API-enabled. It addresses the challenges of older technology from previous vendors that have no API capability. It works on a fully operable backward compatible standard. While this appears simple enough, the ground realities are different and require an experienced team. APIs in healthcare must be created custom to the need of the service it is providing for. The management of APIs for healthcare can get complex if any of the systems are upgraded or replaced.
If you are looking to outsource practice management system development or want to know more about it, feel free to contact us. iTech is an HIPAA compliant organization , located in Addison, Texas with an offshore development center in India. This makes us a cost-effective as well as a reputed name in custom software development.







